ST. LOUIS, Mo. — Although smoking plays a key role in many cases of lung cancer, scientists say some people can still develop lung tumors without ever picking up a cigarette in their lives. A new study has discovered that cases of “never-smokers’” lung cancer are very different from the variety of the disease smokers suffer from. Moreover, these differences have revealed a new treatment method which can cure most cases of never-smokers’ cancer.
A team from Washington University School of Medicine in St. Louis says precision drug treatments which target specific mutations in the lungs of never-smokers can positively impact 78 to 92 percent of these cancer patients. Researchers note that the U.S. Food and Drug Administration has already approved these drugs for use.
What makes never-smokers’ cancer different?
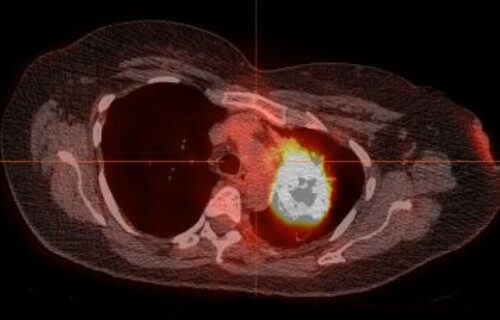
The study reveals that the majority of lung tumors in people who don’t smoke have so-called driver mutations. These are specific errors in a person’s DNA that fuel tumor growth which many drugs can successfully block. Conversely, just half of the tumors in people who smoke tobacco have driver mutations.
“Most genomic studies of lung cancer have focused on patients with a history of tobacco smoking,” says senior author and professor of medicine Ramaswamy Govindan, MD, in a university release.
“And even studies investigating the disease in patients who have never smoked have not looked for specific, actionable mutations in these tumors in a systematic way. We found that the vast majority of these patients have genetic alterations that physicians can treat today with drugs already approved for use. The patient must have a high-quality biopsy to make sure there is enough genetic material to identify key mutations. But testing these patients is critical. There is a high chance such patients will have an actionable mutation that we can go after with specific therapies.”
Overall, just 10 to 15 percent of lung cancer cases in the United States occur in people with no history of smoking. That number is around 40 percent in certain regions of Asia.
Your DNA reveals whether or not you smoke
Researchers examined lung tumor samples from 160 patients with lung adenocarcinoma and no history of smoking tobacco. They compared those patients to data on smokers and never-smokers in the The Cancer Genome Atlas and the Clinical Proteomic Tumor Analysis Consortium — projects which look at different kinds of cancer.
The team confirmed a patient’s non-smoking status by examining the patterns in their mutations and comparing them to the results among lung cancer patients who smoke. Govindan and his team say a smoker’s lung tumors contain about 10 times the number of mutations in comparison to tumors in never-smokers.
“Tobacco smoking leads to characteristic changes in the tumor cells, so we can look for telltale signs of smoking or signs of heavy exposure to secondhand smoke, for example,” Govindan explains. “But very few of these patients’ tumors showed those signs, so we could verify that this was truly a sample of lung cancer tumors in patients who had never smoked or had major exposure to tobacco smoke.”
Are never-smokers born with a higher risk of cancer?
So, what’s causing people who never smoke tobacco to end up with lung tumors? One possibility is that their genes contain factors making them more likely to develop a tumor. However, the study found that only seven percent of never-smokers had mutations present at birth that increase their risk of cancer. Researchers say this discovery only makes never-smokers’ lung cancer even more mysterious.
“There appears to be something unique about lung cancer in people who have never smoked,” Govindan adds. “We didn’t find a major role for inherited mutations, and we don’t see evidence of large numbers of mutations, which would suggest exposure to secondhand smoke. About 60% of these tumors are found in females and 40% in males. Cancer in general is more common among men, but lung cancer in never-smokers, for some unexplained reasons, is more common among women. It is possible additional genes are involved with predispositions to cancers of this kind, and we just don’t know what those are yet.”
While the trigger for never-smokers’ tumors is still unclear, researchers say their findings give doctors new insight into the genetic profile of this disease. It also explains why a type of immunotherapy called checkpoint inhibitors doesn’t work as well on these tumors. Only a small portion of never-smokers’ tumors have immune cells or immune checkpoint molecules which these anti-cancer drugs trigger to fight the disease.
“The most important finding is that we identified actionable mutations in the vast majority of these patients — between 80% and 90%,” Govindan concludes. “Our study highlights the need to obtain high-quality tumor biopsies for clinical genomic testing in these patients, so we can identify the best targeted therapies for their individual tumors.”
The study appears in the Journal of Clinical Oncology.