NEW YORK — The pandemic has been stressful for many Americans, but various racial and economic groups are experiencing the impact of that stress in very different ways, a new study finds.
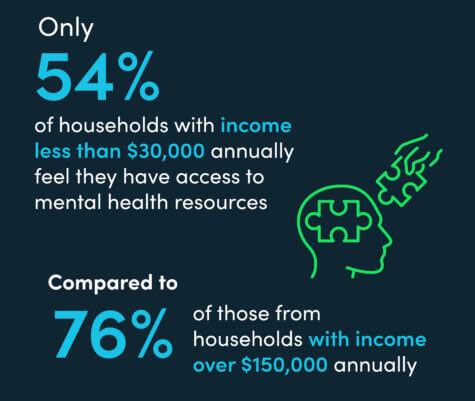
A survey of 2,001 people finds that only 54 percent of those from lower-income households (making less than $30,000 annually) feel they have access to the resources they need to take care of their mental health. That’s in comparison to 76 percent of those from high income households (making $150,000 or more annually).
Conducted by OnePoll on behalf of Big Health, researchers also report that class disparities were also present for those seeking care.
Just 39 percent of those from lower-middle-income households (earning between $30,000 and $59,999 annually) have sought help, compared to 57 percent of high-income earners. In comparison to high-income households, respondents who make less than $30,000 a year were twice as likely to cite expenses as a barrier to professional mental health support.
The most common symptoms include heightened anxiety (64%), feelings of depression (53%), and increased nervousness (50%).
The mental health stigma is still there
 Asian Americans (76%) and African Americans (68%) were the most likely to say they face stigma from their community around seeking help for mental health issues, compared to just 57 percent of white Americans.
Asian Americans (76%) and African Americans (68%) were the most likely to say they face stigma from their community around seeking help for mental health issues, compared to just 57 percent of white Americans.
Americans of Asian and Pacific Islander descent were more than twice as likely (52%) as white Americans (23%) to strongly agree that 2020 was the most stressful year of their lives. African Americans were also likely to list 2020 as the most stressful year of their lives, with 34 percent strongly agreeing with the statement.
“Although we have made significant progress normalizing mental health care, stigma and cost continue to be a significant barrier for those seeking support, especially within underserved populations,” says Big Health Chief Medical Officer Dr. Jenna Carl in a statement. “Moving forward, it is paramount that we focus on improving mental health equity by offering clinically based approaches to those who may not otherwise have access to care.”
Many are ‘self-medicating’ during the pandemic
Feelings of isolation due to lockdowns (57%), being overwhelmed due to constant societal changes (49%), and stress at work (30%) — all common causes of sleep disruption, according to the National Sleep Foundation — are likely leading to longer-term problems.
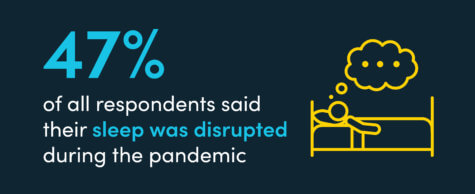 In fact, nearly half of respondents indicated their sleep was disrupted during the pandemic.
In fact, nearly half of respondents indicated their sleep was disrupted during the pandemic.
Respondents often look at prescription medication as a solution — 39 percent are currently taking some form of pill for their mental health.
When prescription medication isn’t an option, some respondents resort to other coping mechanisms; three in 10 claimed to self-medicate, while one in five reportedly use alcohol to deal with their mental health.
“We’ve seen radically increased demand for non-drug alternatives for mental health as a result of the pandemic. If there is a silver lining to the past year and a half, it’s the collective realization that we need to increase access to evidence-based mental health care for those who need it,” adds Big Health Co-founder and CEO Peter Hames.
