Doctors say damage seen in deceased coronavirus patients ‘not consistent with typical heart muscle inflammation patterns.’
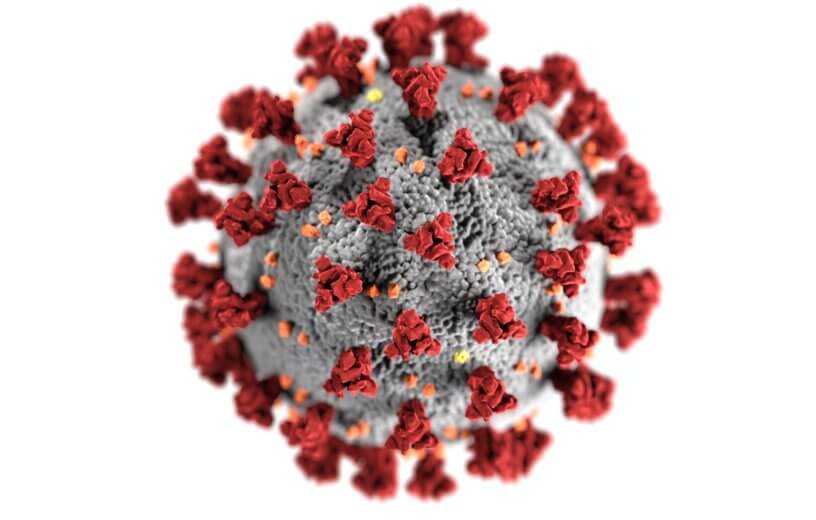
NEW ORLEANS — It’s become quite evident the past few months that COVID-19 can have an adverse effect on the heart. Still, scientists and doctors are still struggling to fully understand the relationship between COVID-19 and heart health. Now, a series of autopsies performed by Louisiana State University pathologists yield some unusual observations.
The team at LSU says that the damage done to the hearts of COVID-19 patients is not consistent with typical heart muscle inflammation patterns seen with myocarditis (heart muscle inflammation). Instead, the observed pattern of cell death is quite unique, and spread across scattered, individual heart muscle cells.
“We identified key gross and microscopic changes that challenge the notion that typical myocarditis is present in severe SARS-CoV-2 infection,” says Dr. Richard Vander Heide, professor and Director of Pathology Research at LSU Health New Orleans School of Medicine, in a release. “While the mechanism of cardiac injury in COVID-19 is unknown, we propose several theories that bear further investigation that will lead to greater understanding and potential treatment interventions.”
Additionally, the pathologists also note SARS-CoV-2 was not present in any heart muscle cells. This is especially odd because the first SARS coronavirus from 2003 was found within the heart muscle cells of SARS patients.
COVID-19 patients also showed no signs of blood vessel blockages in their coronary arteries.
‘Extreme stress on heart’
A total of 22 autopsies are included in this study. All of those patients had passed away due to COVID-19 while being treated at the University Medical Center in New Orleans. Most of the patients are African-American, with 10 being male and 12 being female. Their ages range from middle age (44 years old) to elderly (79). Most had preexisting high blood pressure, half had type 2 diabetes, and 41% were obese.
So, what was found? Diffuse alveolar damage (DAD), or damage to the small lung airspaces that facilitate the exchange of gas, was observed among the autopsied patients. Also, both blood clots and bleeding were seen in the blood vessels and capillaries of the lungs. All of these factors were determined to be major contributors to the patients’ deaths.
CLICK HERE TO SUBSCRIBE TO OUR NEWSLETTER & GET THE LATEST STUDIES FROM STUDYFINDS.ORG BY EMAIL!
“These findings, along with severely enlarged right ventricles, may indicate extreme stress on the heart secondary to acute pulmonary disease,” says Dr. Sharon Fox, Associate Director of Research and Development in the Department of Pathology at the school.
Pathologists also point to viral infections among cells in the lining of the smaller blood vessels (endothelium) of patients. While these infections were at relatively “low levels,” the team at LSU theorize it may have been enough to induce individual cell death.
The “cytokine storm,” or overreaction of the immune system to the infection, may also contribute to these observations.
“Given that inflammatory cells can pass through the heart without being present in the tissue proper, a role for cytokine-induced endothelial damage cannot be ruled out,” Dr. Heide concludes.
The study is published in Circulation.
Like studies? Follow us on Facebook!