PHILADELPHIA — Any mental illness can be debilitating, but schizophrenia stands out as an especially scary mental disorder. Characterized by hallucinations, irrational thoughts, and losing touch with reality, schizophrenia is an illness that still raises more questions than modern medicine has answers. Now, researchers at the University of Pennsylvania Medical School have made a potentially groundbreaking discovery. For the first time ever, two distinct neuroanatomical variations of schizophrenia have been identified.
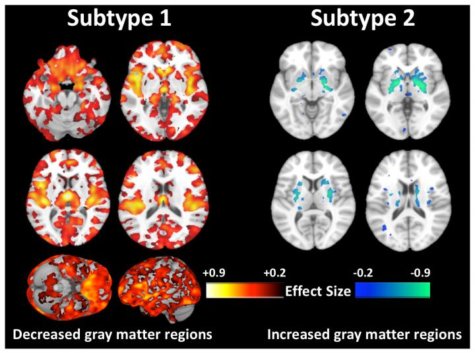
Researchers analyzed the brain scans of over 300 schizophrenia patients to make their discovery. The first variation shows lower volumes of gray matter in comparison to a healthy brain. The second type of schizophrenia, though, shows largely the same levels of gray matter that would be seen in a normal brain scan. Needless to say, these findings may revolutionize mankind’s understanding of schizophrenia, as well as identification and treatment methods.
“Numerous other studies have shown that people with schizophrenia have significantly smaller volumes of brain tissue than healthy controls. However, for at least a third of patients we looked at, this was not the case at all — their brains were almost completely normal,” says principal investigator Christos Davatzikos, PhD, in a release. “In the future, we’re not going to be saying, ‘This patient has schizophrenia,’ We’re going to be saying, ‘This patient has this subtype’ or ‘this abnormal pattern,’ rather than having a wide umbrella under which everyone is categorized.”
As mentioned before, schizophrenia is a disorder that still puzzles doctors, and most previous attempts at studying its impact on the brain have been centered on comparing healthy brains to scans performed on patients diagnosed with schizophrenia. Now, with this new discovery in mind, it’s clear why this approach wasn’t proving to be effective.
Davatzikos research for this study spanned three nations (United States, China, Germany), and encompassed 307 schizophrenia patients as well as 364 healthy participants as a control group. All study participants were 45-years old or younger.
After all the brain scans were taken, the research team used an advanced machine learning method (developed at UPenn) called HYDRA. Without getting into the intricacies of the approach, this allowed them to mitigate the influence of any outside variables and identify “true disease subtypes.”
“This method enabled us to sub-categorize patients and find how they differed from the controls, while allowing us, at the same time, to dissect this heterogeneity and tease out multiple pathologies, rather than trying to find a dominant pattern,” Davatzikos says.
Astoundingly, the study’s authors discovered that 155 (40%) of the schizophrenia patients’ brain scans didn’t show the typical pattern of diminished gray matter volume that’s been accepted for decades as how schizophrenia manifests itself in the mind. These schizophrenia patients’ brains actually showed increased brain volume in the middle of the brain. That middle portion is called the striatum and it helps control one’s movement. The researchers still don’t have an explanation for these observations.
“The subtype 2 patients are very interesting, because they have similar demographic and clinical measures with subtype 1, and the only differences were their brain structures,” comments co-lead author Ganesh Chand, PhD, postdoctoral researcher in the radiology department at Penn.
There are a number of antipsychotic medications currently available for schizophrenia patients, but their effectiveness varies greatly.
“The treatments for schizophrenia work really well in a minority of people, pretty well in most people, and hardly at all in a minority of people. We mostly can’t predict that outcome, so it becomes a matter of trial and error,” Wolf explains. “Now that we are starting to understand the biology behind this disorder, then we will hopefully one day have more informed, personalized approaches to treatment.”
As far as why an entire group of schizophrenia patients’ brains appear very similar to those of healthy individuals, Davatzikos is at a loss.
“This is where we are puzzled right now,” he concludes. “We don’t know. What we do know is that studies that are putting all schizophrenia patients in one group, when seeking associations with response to treatment or clinical measures, might not be using the best approach.”
Naturally, Davatzikos and his team are already planning further, more comprehensive research into this matter in pursuit of answers.
The study is published in Brain.